The Food and Drug Administration (FDA) recently announced a significant change in its COVID-19 vaccine approval policies, focusing primarily on older Americans and those deemed “high-risk.” This shift aims to establish more stringent standards for low-risk individuals seeking vaccination. According to the FDA, this new approach is anticipated to be rolled out for the upcoming fall vaccination season, with an emphasis on clear, scientific data to support the recommendations, marking a departure from the previous broad vaccine access model.
| Article Subheadings |
|---|
| 1) Details of the FDA’s New Vaccine Approval Criteria |
| 2) Impact on High-Risk Individuals |
| 3) Transition from Universal Approach to Targeted Policies |
| 4) Challenges in Public Trust and Acceptance |
| 5) Future Directions for COVID-19 Vaccination Policies |
Details of the FDA’s New Vaccine Approval Criteria
The FDA has stated that its revised policy will center on vaccinating Americans aged 65 and older, along with those at high risk of severe complications from COVID-19. According to officials, those in low-risk categories will face stricter scientific scrutiny regarding vaccine approvals. This significant change is designed to ensure that comprehensive data is collected and analyzed before any vaccinations are approved for individuals who are less likely to suffer severe effects from the virus. The policymakers estimate that between 100 million to 200 million Americans can expect access to these vaccines, particularly targeting older adults.
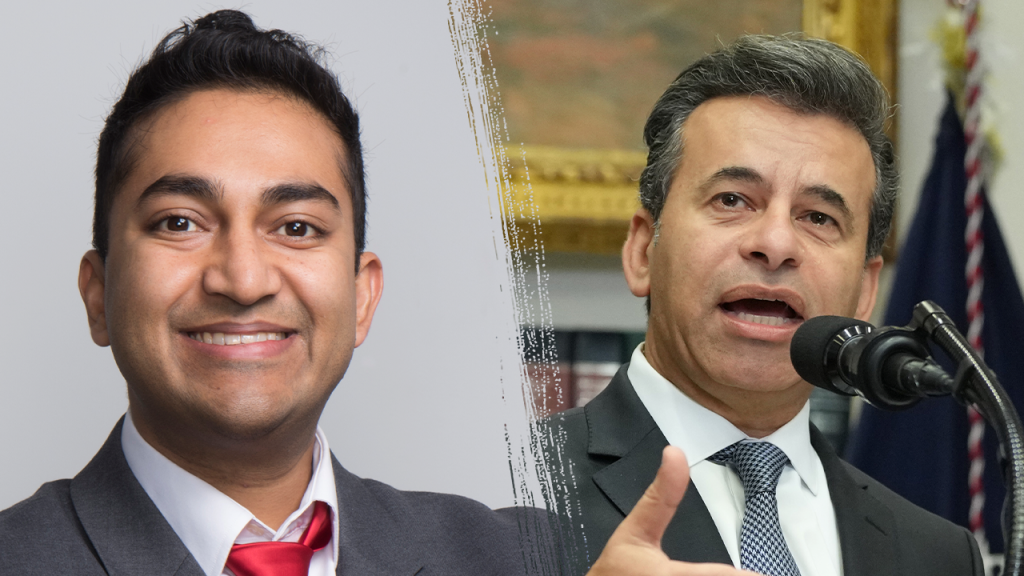
The FDA’s leaders, including the Center for Biologics Evaluation and Research chief, Vinay Prasad, and FDA Commissioner Martin Makary, have emphasized the need for a heightened standard of evidence. They noted that clinical trials would not only shape future FDA directions but also capably inform healthcare providers and the American public about vaccine efficacy and safety. As they write in their publication, these measures are in direct response to demands for clarity and robust data.
Impact on High-Risk Individuals
The newly outlined policies are poised to particularly benefit Americans who fall within the high-risk category, including older adults and individuals with specific health conditions. This targeted approach is likely to ensure that those who genuinely need the protection offered by vaccines receive it promptly and efficiently. As the FDA shifts its focus to high-risk individuals, it aims to reduce the complications that arise when low-risk individuals flood vaccine distributions, which can lead to overcrowding and resource allocation issues.
Moreover, by streamlining vaccine approvals for high-risk groups, the FDA hopes to enhance overall public health outcomes, reducing the incidence of severe cases among the population that is most vulnerable. This shift reflects an evolution in thinking about public health interventions where the most critical needs are addressed first, potentially stabilizing hospital systems more rapidly and ensuring that the capacities are in place to handle surges in cases.
Transition from Universal Approach to Targeted Policies
The FDA’s decision to abandon the previous “one-size-fits-all” approach is notable, especially considering that many other high-income nations have adopted similar policies geared towards older and high-risk populations. Experts argue that the U.S. has been slower to respond to these dynamics, relying instead on broad marketing authorizations that applied to the general public without adequate scrutiny.
“While all other high-income nations confine vaccine recommendations to older adults or those at high risk for severe Covid-19, the United States has granted broad marketing authorization to all Americans over the age of 6 months,”
indicated the FDA leaders in their article.
This transition is not merely a response to internal demands but also aligns U.S. policies more closely with established guidelines from European nations. As outlined in their discourse, this shift not only improves healthcare resource management but also enhances communication and clarity surrounding vaccine protocols, ultimately diminishing confusion among the public.
Challenges in Public Trust and Acceptance
Despite these efforts, gaining public trust poses a considerable challenge. Recent polls and studies show a notable decline in trust towards institutions like the FDA. The pandemic has left many individuals skeptical about the integrity and efficacy of medical recommendations.
“Survey after survey shows trust in institutions like the FDA and scientists in general, it’s rock bottom,”
Prasad remarked during a roundtable discussion. The necessity to regain public confidence is critical, especially with ongoing debates surrounding vaccine hesitancy, highlighted by contrasting opinions on the number of recommended booster shots.
Prasad’s observation about the divided nature of opinions reflects a broader societal dilemma. Some members of the public expressed concerns about the regulatory process and the safety of COVID-19 vaccines, while others continue to seek out protection through vaccination. This disparity has resulted in low uptake rates for recommended vaccines.
Future Directions for COVID-19 Vaccination Policies
The FDA anticipates that by elevating the standards for vaccine approvals, it can rebuild trust and improve public acceptance. The policy shift encourages calls for increased transparency and open discussion about vaccination safety and efficacy. The ultimate goal is to create a well-informed public that comprehends the reasons behind the targeted approach to vaccine distribution.
Going forward, the FDA will require manufacturers to gather extensive clinical trial data to validate the rollout of any new COVID-19 vaccine aimed at low-risk populations. Strengthening the data collection process not only adheres to transparency but also reassures the public that their concerns are acknowledged. As vaccines continue to evolve, the FDA aims to institute a more adaptive and scientifically grounded framework that resonates with the American public’s needs and expectations.
| No. | Key Points |
|---|---|
| 1 | FDA shifts focus to prioritize COVID-19 vaccinations for individuals over 65 and high-risk groups. |
| 2 | Stricter approval processes will be implemented for low-risk individuals seeking vaccination. |
| 3 | The approach aligns more closely with guidelines established in other high-income nations. |
| 4 | Public trust in healthcare institutions has significantly declined since the COVID-19 pandemic. |
| 5 | FDA aims to rebuild public confidence through transparent communication and rigorous data collection. |
Summary
The FDA’s recent policy changes signal a drastic shift in COVID-19 vaccination strategies, emphasizing evidence-based guidelines for high-risk populations while demanding greater scrutiny for low-risk individuals. This transition aims not only to enhance public health outcomes but also to restore trust in health institutions that have faced skepticism due to previous regulatory approaches. As the country prepares for the upcoming vaccination season, these efforts reflect a growing recognition of the need for tailored healthcare solutions.
Frequently Asked Questions
Question: Why is the FDA focusing on older individuals and high-risk populations for COVID-19 vaccinations?
The FDA believes that targeting older individuals and those at higher risk of severe COVID-19 complications will enhance the effectiveness of vaccination programs and ensure those most vulnerable receive timely protection.
Question: What changes will occur regarding the approval of vaccines for low-risk individuals?
The FDA plans to implement stricter requirements for clinical trial data to ensure that any vaccines recommended for low-risk individuals are thoroughly evaluated for safety and efficacy.
Question: How can the FDA rebuild public trust in vaccination programs?
By emphasizing transparency, engaging in open discussions about vaccine safety, and addressing public concerns, the FDA aims to re-establish confidence among the public regarding vaccination policies and health guidelines.