A recent study has highlighted alarming trends in childhood measles vaccination rates across the United States, revealing significant disparities at the county level. Published by researchers at Johns Hopkins University, the study documented a decrease in vaccination coverage from the 2017-2018 school year to the 2023-2024 school year. As the nation grapples with a notable resurgence of measles cases, officials are calling for targeted interventions to improve vaccination rates and safeguard public health.
| Article Subheadings |
|---|
| 1) Overview of Vaccination Decline |
| 2) County-Level Vaccination Data |
| 3) The Measles Outbreak |
| 4) Vulnerable Areas and Herd Immunity |
| 5) Future Considerations and Public Health Strategy |
Overview of Vaccination Decline
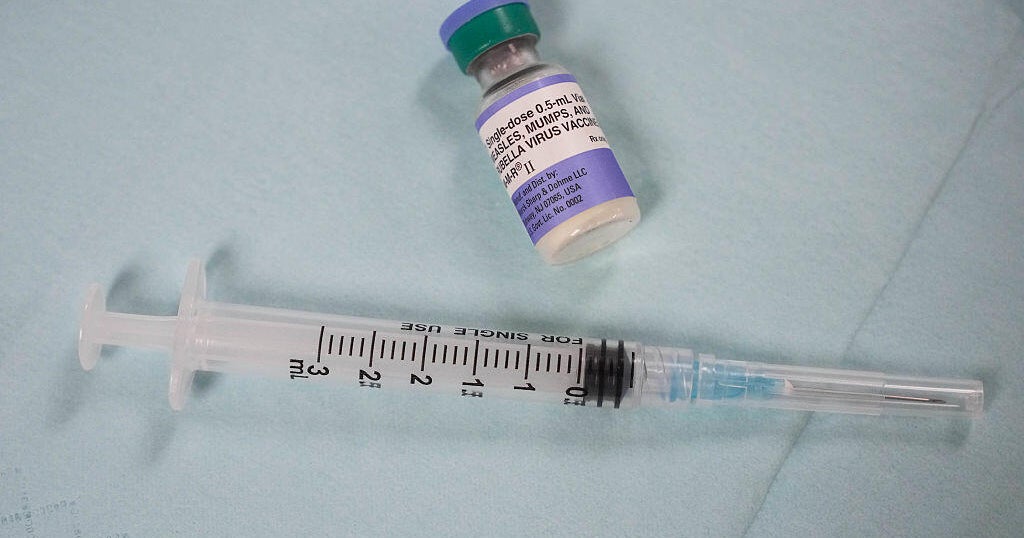
Vaccination rates for childhood diseases have faced substantial declines since the onset of the COVID-19 pandemic, a phenomenon observed in various public health reports. According to the Johns Hopkins University study, the MMR (measles, mumps, and rubella) vaccination rate decreased from an impressive 93.92% in the 2017-2018 school year to a concerning 91.26% in the 2023-2024 school year. The reduction in vaccination coverage raises alarms among pediatricians and public health experts who argue that maintaining high vaccination rates is crucial for preventing outbreaks of infectious diseases.
The researchers focused on data from 33 states, excluding others due to missing vaccination information. The findings indicated that the decline is not uniform across the nation, suggesting complex socio-economic and geographic factors affecting vaccination uptake. With such a critical drop, health officials are increasingly worried that the potential for disease transmission has risen drastically, emphasizing the need for concerted health education and outreach initiatives aimed at families.
County-Level Vaccination Data
The study surveyed 2,066 counties within the 33 states and found that an alarming 78% experienced a decline in vaccination rates. Interestingly, only four states—namely, California, Connecticut, Maine, and New York—reported an increase in average county-level vaccination rates. This disparity highlights a significant variation in public health responses and community readiness to combat vaccine hesitancy.
These findings prove crucial for formulating targeted public health strategies. The data allows health officials to identify specific counties and communities that require immediate attention and resources to improve vaccination coverage. By mapping these trends, experts can better tailor interventions that resonate with families and community leaders, ultimately reinforcing the importance of immunization in safeguarding child health.
The Measles Outbreak
The report coincided with what has been described as the largest measles outbreak in the U.S. since the 2019 wave, with the Centers for Disease Control and Prevention (CDC) reporting 1,088 cases nationwide as of the end of May. Notably, the majority of these cases are concentrated in West Texas, posing a significant public health challenge. Health experts emphasize that the outbreak is particularly concerning given the historical context, as vaccination campaigns have successfully controlled measles for decades.
The CDC reported that among the reported cases, 96% involve individuals who are either unvaccinated or whose vaccination status is unknown. The highly contagious nature of measles means that unprotected individuals are at an elevated risk of severe health complications, including pneumonia and, in rare instances, death. In light of recent outbreaks, officials warn of the broader implications and long-lasting effects low vaccination coverage could have on public health.
Vulnerable Areas and Herd Immunity
Health professionals are increasingly concerned about regions with particularly low vaccination rates, which reflect vulnerabilities to outbreaks. For instance, counties like Gaines County in West Texas, where vaccination rates hover around 80%, exemplify this heightened risk. Such areas have been flagged by experts as epicenters for the ongoing measles outbreak, highlighting the necessity for local health departments to prioritize vaccination drives and community education.
Achieving herd immunity—defined as the threshold at which over 95% of a population is vaccinated—is critical in preventing disease transmission. However, many counties across the nation are falling short of this benchmark. As health experts note, these vulnerabilities create fertile ground for the resurgence of diseases that were once under control, leading to potential public health crises.
Future Considerations and Public Health Strategy
In response to the alarming decline in vaccination rates and the ongoing measles outbreak, public health advocates stress the need for immediate and effective intervention strategies. This includes leveraging data to identify high-risk communities and organizing localized vaccination campaigns. Health officials aim to collaborate with schools, community organizations, and families to foster a better understanding of the importance of vaccinations and to address common concerns and misconceptions.
Furthermore, continuous monitoring of vaccination rates and disease outbreaks will be crucial for evaluating the effectiveness of these strategies. Public health campaigns should also incorporate outreach tailored to cultural and socio-economic contexts to enhance community participation and trust. Health departments must recommit to fighting misinformation surrounding vaccines to ensure public confidence in vaccination programs.
| No. | Key Points |
|---|---|
| 1 | Vaccination rates for childhood diseases have significantly declined since the COVID-19 pandemic. |
| 2 | A study found that 78% of the counties surveyed experienced a decline in MMR vaccination rates. |
| 3 | The ongoing measles outbreak has revealed the risks posed by low vaccination coverage in certain regions. |
| 4 | Herd immunity is critical but remains unachieved in many communities across the U.S. |
| 5 | Public health efforts must include targeted outreach and education to raise vaccination rates. |
Summary
The decline in childhood vaccination rates, as evidenced by the recent Johns Hopkins University study, poses serious public health risks, particularly in the context of rising measles outbreaks across the United States. The disparities in vaccination coverage underline the need for targeted public health strategies that prioritize high-risk communities. Policymakers and health officials must work collaboratively to address misinformation and implement effective vaccination campaigns to ensure the safety and well-being of children nationwide.
Frequently Asked Questions
Question: What are the implications of low vaccination rates?
Low vaccination rates can lead to increased outbreaks of preventable diseases, heightened healthcare costs, and more severe health complications for unvaccinated individuals.
Question: How can communities improve vaccination rates?
Communities can enhance vaccination rates through targeted outreach programs, educational campaigns, and partnerships with schools and local organizations to foster trust in vaccines.
Question: What is herd immunity?
Herd immunity occurs when a high percentage of a community is vaccinated, thus providing protection for those who are unable to be vaccinated, effectively reducing disease transmission.