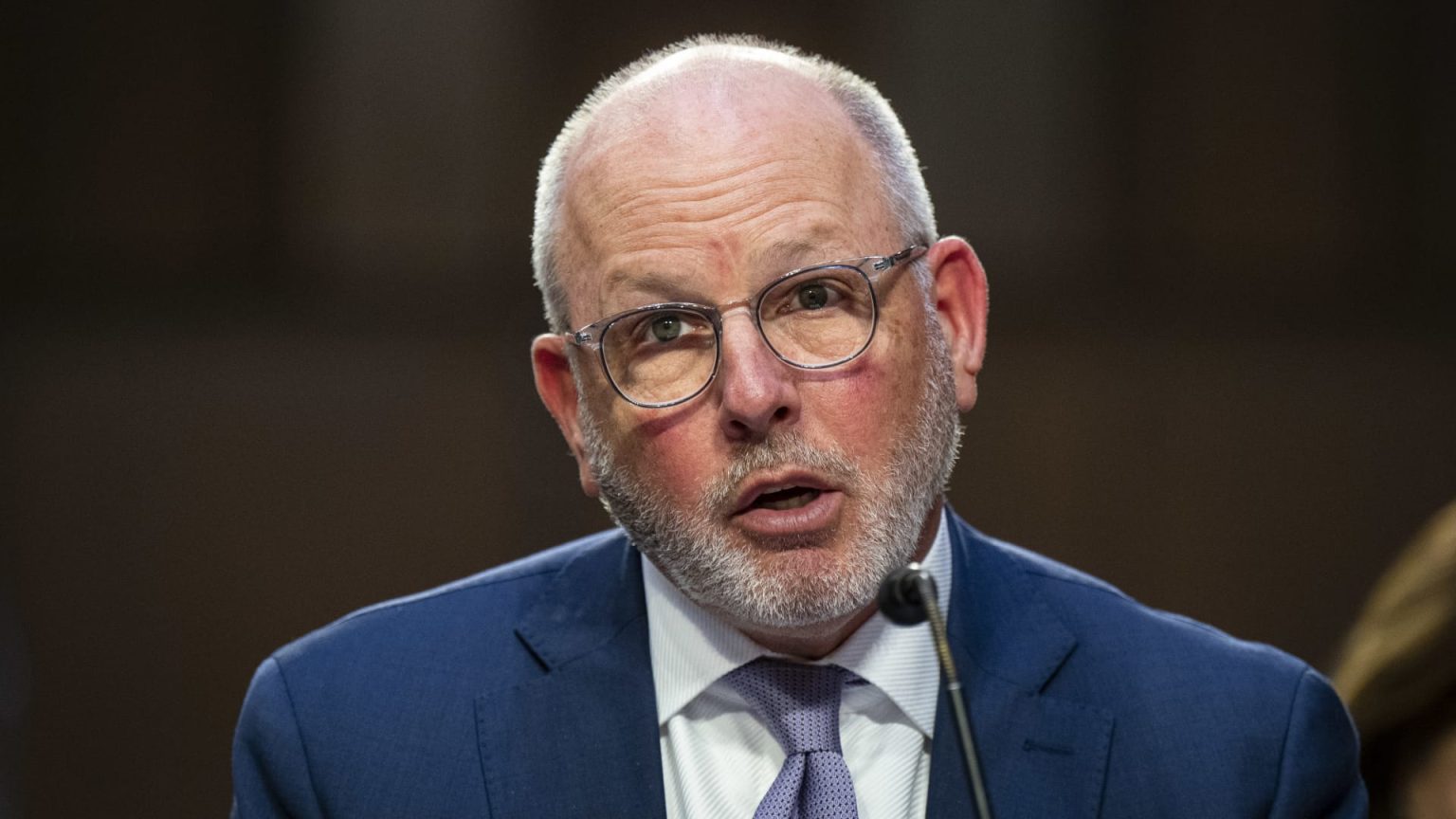
In a recent Senate hearing, David Joyner, the newly appointed CEO of CVS Health, vehemently defended the role of pharmacy benefit managers (PBMs), particularly his company’s Caremark unit, amidst ongoing scrutiny concerning rising drug prices in the United States. Joyner’s statements came at a pivotal moment as lawmakers and various stakeholders call for stronger regulations on PBMs, attributing significant blame for the escalating costs of prescription medications. During his address, he challenged the accusations against PBMs, shifting focus toward the pharmaceutical manufacturers whom he claims are responsible for maintaining high drug prices due to monopolistic practices.
| Article Subheadings |
|---|
| 1) Overview of Pharmacy Benefit Managers and Their Role |
| 2) Recent Senate Hearing and Key Takeaways |
| 3) Joyner’s Defense and Economic Claims |
| 4) Industry Reactions and Challenges Ahead for PBMs |
| 5) The Future of Drug Pricing and Legislative Implications |
Overview of Pharmacy Benefit Managers and Their Role
Pharmacy benefit managers (PBMs) serve as intermediaries between insurers, drug manufacturers, and pharmacies to manage prescription drug benefits. These entities negotiate discounts and rebates with pharmaceutical companies and determine the formularies, or lists of covered medications, that insurers will provide to their beneficiaries. While this system is designed to lower costs for health plans and patients alike, PBMs have faced intense backlash for allegedly increasing prices rather than passing savings directly onto consumers. Their influence in the U.S. healthcare system is significant, as it is reported that PBMs collectively administer about 80% of the prescriptions filled in the country.
The relationship between PBMs and the overall drug supply chain is crucial, as the actions of these managers can have a direct impact on both the pricing of drugs and patient access to medications. Proponents argue that by negotiating on behalf of insurers, PBMs are essential in lowering the overall costs of healthcare, while critics contend that they contribute to the inflated pricing structure by prioritizing profits over patient needs.
Recent Senate Hearing and Key Takeaways
During a Senate Health, Education, Labor, and Pensions Committee hearing held on May 10, 2023, David Joyner took the opportunity to respond to claims made against PBMs. His testimony was particularly notable as it unfolded in an environment where political pressure was mounting from both sides of the aisle to evaluate and potentially reform the practices of these middlemen. Joyner’s remarks marked a significant moment in CVS’s communication strategy, as it emphasized the company’s stance on ongoing accusations that PBMs contribute to rising drug prices. Notably, various government officials, including the President, have expressed interest in the operations of PBMs, highlighting the growing concern over their financial practices.
Joyner focused heavily on outlining the role of Caremark, CVS’s PBM subsidiary, in the context of rising healthcare costs, attempting to reposition the narrative from blame to contribution. His remarks reflected an understanding that the scrutiny of PBMs has reached policy levels, affecting public perception and necessitating a robust defense from industry leaders.
Joyner’s Defense and Economic Claims
In his testimony, David Joyner presented an assertive defense of the Caremark unit, stating that PBMs are crucial in offsetting healthcare costs. Joyner noted that the rising costs are attributed to several factors, including increased patient utilization of services, heightened expenses from healthcare providers, labor shortages, and significant price increases for brand-name drugs. He mentioned that manufacturers have contributed to an annual gross drug spending increase estimated at $21 billion just from price hikes occurring in the first three weeks of the year.
Moreover, Joyner cited that PBMs like Caremark play an essential role in managing the complex drug supply chain and contribute significantly to the overall healthcare system, claiming they generate net savings exceeding $100 billion annually. He asserted,
“Our work is a critical counterbalance to the monopolistic tendencies of drug manufacturers.”
This comment underscores his belief in the necessity of PBMs as a preventive measure against the monopolistic pricing strategies of pharmaceutical companies.
Industry Reactions and Challenges Ahead for PBMs
The reaction to Joyner’s statements from the pharmaceutical industry was immediate and pointed. The Pharmaceutical Research and Manufacturers of America (PhRMA), a prominent lobbying group for drug manufacturers, issued a statement agreeing that PBMs are “under intense, well-deserved scrutiny.” They emphasized that bipartisan state attorneys general and various legislators are investigating the roles and impacts of PBMs on drug pricing.
PhRMA raised concerns that PBMs often pocket the savings gained from negotiated rebates instead of passing them onto consumers, suggesting a conflict of interest in their dual roles of cost negotiator and profit generator. This tension reflects a growing mistrust among stakeholders, including healthcare providers, insurers, and patients, which complicates the operational landscape for PBMs and poses significant challenges as regulators consider reforms.
The Future of Drug Pricing and Legislative Implications
Looking forward, the debate surrounding drug pricing is expected to intensify, with potential legislative reforms aimed directly at the operations of PBMs on the horizon. Lawmakers across the political spectrum are seeking to address the complexities of drug pricing and the role of intermediaries in maintaining a system many argue prioritizes corporate profits over patient care. As investigations continue and public outrage grows, it is likely that PBMs will face tighter regulations and increased transparency requirements.
As the landscape evolves, the effectiveness of PBMs will be scrutinized more than ever, requiring them to adapt to ensure they can demonstrate value in a system increasingly viewed with skepticism. The outcome of this scrutiny will have lasting implications for the healthcare industry and its stakeholders.
| No. | Key Points |
|---|---|
| 1 | CVS Health’s CEO, David Joyner, defended PBMs, claiming they help mitigate rising healthcare costs. |
| 2 | Joyner shifted blame for high drug prices towards pharmaceutical manufacturers and their pricing strategies. |
| 3 | The Senate hearing revealed bipartisan concerns regarding the operations of PBMs and their pricing effects. |
| 4 | Pharmaceutical industry lobbies, such as PhRMA, critiqued PBM operations, emphasizing the need for more scrutiny. |
| 5 | Future legislative reforms focusing on PBMs may occur as investigations into their practices intensify. |
Summary
The discussions around pharmacy benefit managers, particularly in light of David Joyner‘s defense at the Senate hearing, underscore the complexities of healthcare pricing in the United States. As tensions rise between pharmaceutical manufacturers and PBMs, the need for clarity and reform in the system becomes increasingly essential. The coming months promise significant developments that may reshape the landscape of drug pricing and accessibility, reflecting the growing emphasis on transparency and accountability within this vital sector of the healthcare system.
Frequently Asked Questions
Question: What are pharmacy benefit managers (PBMs)?
Pharmacy benefit managers (PBMs) are intermediaries that manage prescription drug benefits for health insurers, negotiating prices and managing formularies to influence the supply chain of medications.
Question: Why are PBMs criticized?
PBMs are criticized for contributing to higher drug prices, as they are accused of not passing on negotiated savings to consumers and prioritizing profits over patient welfare.
Question: What might the future hold for PBMs?
The future for PBMs is uncertain as increasing scrutiny and potential legislative reforms could alter their operational landscape, leading to greater transparency and accountability in drug pricing practices.