In a significant development for the weight loss market, CVS Health has announced an expansion of access to the drug Wegovy, a popular obesity treatment, through its pharmacy benefit manager, Caremark. This initiative is set to take effect on July 1, with Wegovy becoming the prioritized GLP-1 drug for patients insured by Caremark. In a corresponding move, the weight loss medication Zepbound will be removed from Caremark’s standard formularies, marking a competitive shift in the market.
| Article Subheadings |
|---|
| 1) Expansion of Wegovy Access |
| 2) Impact on Competing Drug |
| 3) Cost and Coverage Details |
| 4) Additional Support Services |
| 5) Future Implications for Patients and Stakeholders |
Expansion of Wegovy Access
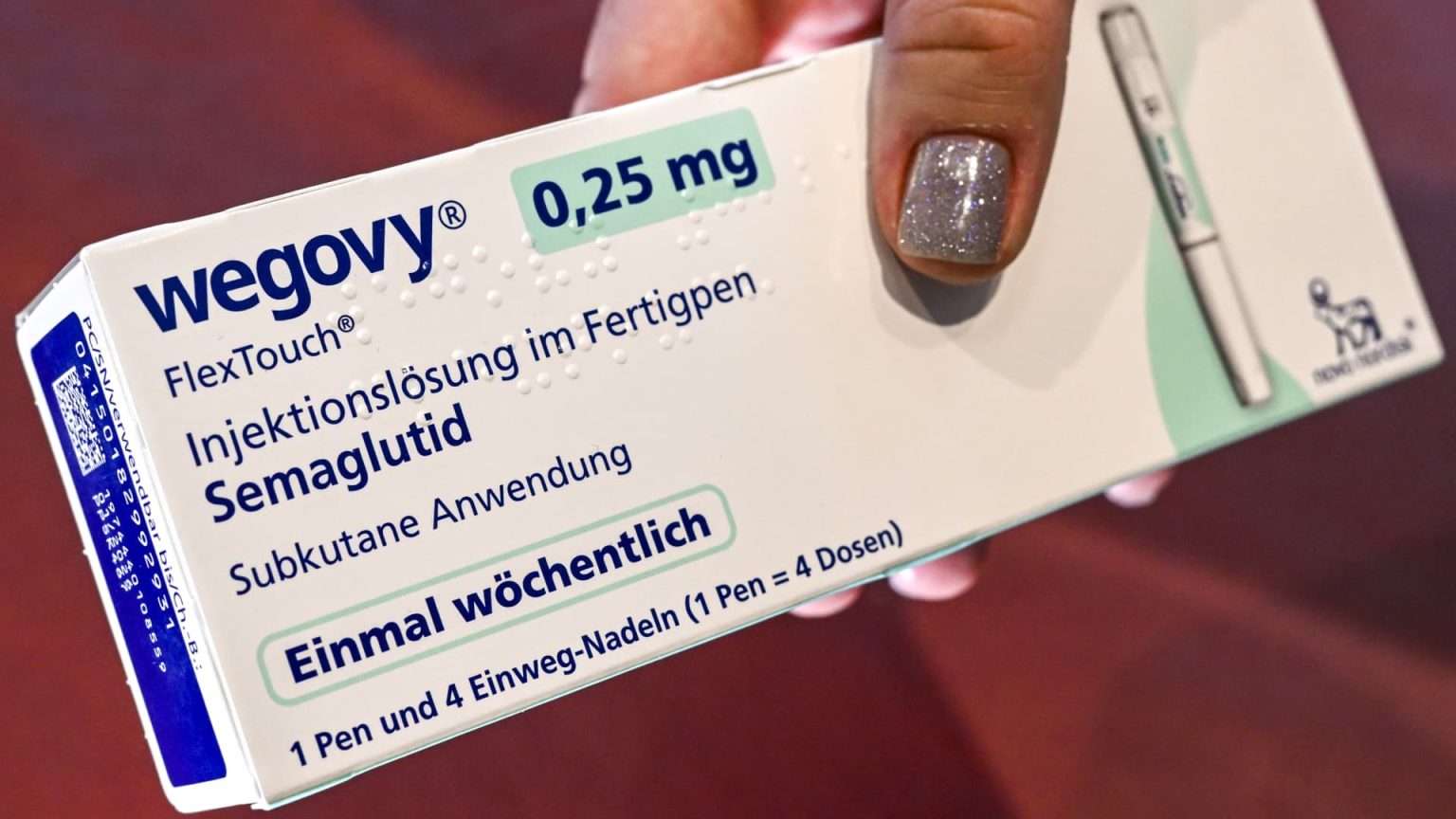
CVS Health has reported that starting July 1, its pharmacy benefit manager, Caremark, will enhance patient access to Wegovy, a leading medication for weight loss. The decision is based on a new partnership with Wegovy’s manufacturer, Novo Nordisk, which underscores CVS’s commitment to providing effective weight management solutions. The prioritization of Wegovy on Caremark’s formularies is expected to facilitate easier access for the millions of patients covered by Caremark, consolidating Wegovy’s position as a preference over alternative obesity treatments.
Officials from CVS stated that this move could significantly benefit patients who have struggled with obesity, providing a medically approved option that aids in weight management. Given the growing public health concern surrounding obesity, the expansion should come as welcome news for those seeking viable treatment options. By aligning its formularies to favor Wegovy, CVS aims to streamline the prescription process for eligible patients.
Impact on Competing Drug
With Wegovy gaining preferential status, Caremark will simultaneously remove the competing medication Zepbound from its standard formularies. This decision is anticipated to have a noticeable financial impact on the manufacturer of Zepbound, Eli Lilly. A recent report indicated that shares of Eli Lilly experienced a significant decline, closing more than 11% lower following the announcement. Analysts are now watching closely to see how this competitive shift will influence the broader market dynamics for weight loss medications.
The implications of this decision extend beyond stock prices; they also reflect changing consumer preferences and competitive strategies among pharmaceutical companies. With Wegovy being favored, it remains to be seen how Eli Lilly will respond, particularly regarding pricing strategies and marketing efforts for Zepbound in the coming months.
Cost and Coverage Details
CVS Health has indicated that eligible patients covered by Caremark will benefit financially from switching to Wegovy. The pharmacy benefit manager has negotiated a more favorable net pricing structure for Wegovy compared to Zepbound, potentially resulting in savings for clients who choose these plans. However, the extent of these savings will ultimately be determined by Caremark’s clients, which include various employers and unions.
These entities will decide how the savings from the lower price of Wegovy will be shared with their members, potentially translating into reduced premiums or lower copayments at pharmacies. Furthermore, for patients who are uninsured or cannot access Wegovy through insurance, CVS offers the drug for $499 out-of-pocket at its 9,000 pharmacies nationwide. This price tag, while steep, remains a viable option for individuals unable to secure insurance coverage.
Additional Support Services
In addition to expanding access to Wegovy, CVS Health has also announced complementary support services as part of its CVS Weight Management program. This initiative will include personalized nutrition plans and other lifestyle aids aimed at helping patients maintain effective weight loss. By offering these additional resources, CVS aims to enhance the overall efficacy of Wegovy as a treatment for obesity.
The integration of lifestyle support aligns with a broader trend in healthcare to provide holistic treatment options. Patients will not only have access to medication but also obtain guidance on lifestyle changes that can significantly impact long-term health outcomes. This comprehensive approach may prove particularly beneficial as healthcare providers increasingly recognize the importance of addressing the multifaceted aspects of weight management.
Future Implications for Patients and Stakeholders
As the obesity treatment landscape continues to evolve, the partnership between CVS Health and Novo Nordisk may serve as a blueprint for future collaborations. Caremark’s decision to prioritize Wegovy comes amidst restrictions on compounding pharmacies, which have been limited in their capacity to produce cheaper, unapproved versions of the drug.
Industry experts believe that this initiative could allow Novo Nordisk to capture a larger share of the market as it looks to improve patient accessibility. Furthermore, Dave Moore, executive vice president of U.S. operations at Novo Nordisk, has stated the company’s commitment to working alongside other stakeholders in the healthcare system to ensure that patients receive proper access to authentic, FDA-approved medications.
Going forward, the successful execution of this partnership could significantly alter patient experiences and options for weight loss treatments. As one of the largest pharmacy benefit managers in the nation, Caremark’s influence in streamlining the procurement of Wegovy may improve healthcare outcomes for patients struggling with obesity.
| No. | Key Points |
|---|---|
| 1 | CVS Health is enhancing access to Wegovy through its Caremark network. |
| 2 | Zepbound will be removed from Caremark’s formularies, affecting its market position. |
| 3 | Caremark has negotiated a lower price for Wegovy compared to its competitor. |
| 4 | CVS is offering additional lifestyle support to complement Wegovy treatment. |
| 5 | The partnership could significantly improve access and impact healthcare outcomes for patients. |
Summary
The announcement by CVS Health to prioritize Wegovy marks a pivotal shift in the obesity treatment landscape. As the drug manufacturer, Novo Nordisk, seeks to capitalize on the growing demand for effective weight management solutions, the partnership illustrates a commitment to patient accessibility and improved health outcomes. With significant changes in drug formularies and the addition of supportive services, this initiative is set to potentially redefine the way obesity treatments are managed and dispensed in the United States.
Frequently Asked Questions
Question: What is Wegovy?
Wegovy is a prescription medication that has been approved for chronic weight management in adults with obesity or overweight conditions.
Question: How does Caremark affect access to medications like Wegovy?
Caremark, as a pharmacy benefit manager, negotiates drug prices and creates formularies that determine which medications are covered for patients based on their insurance plans.
Question: What kind of support services does CVS offer alongside Wegovy?
CVS provides additional services, including personalized nutrition plans and lifestyle support, to enhance the effectiveness of Wegovy treatments for managing weight.