A significant spike in hepatitis A cases has been reported in four European countries, alarming health officials. Between January and May 2025, Austria, Czechia, Hungary, and Slovakia saw a collective total of 2,097 infections, leading to several deaths. The European Centre for Disease Prevention and Control (ECDC) has issued a rapid risk assessment to address this ongoing public health crisis, highlighting the need for increased vaccination and sanitation efforts.
| Article Subheadings |
|---|
| 1) Current State of Hepatitis A Cases |
| 2) Understanding Hepatitis A |
| 3) At-Risk Populations |
| 4) Response Measures by Health Authorities |
| 5) The Importance of Vaccination and Awareness |
Current State of Hepatitis A Cases
As reported by the European Centre for Disease Prevention and Control (ECDC), a total of 2,097 cases of hepatitis A have been documented between January and May 2025 across Austria, Czechia, Hungary, and Slovakia. The majority of cases have emerged from Slovakia, which has been grappling with an active outbreak since 2022; here, 880 infections have been noted. Czechia follows closely, with 600 cases reported along with six fatalities attributed to the disease.
Hungary has recorded 530 cases in the same timeframe, while Austria has seen 87 cases. The ECDC’s assessment outlines the urgent need for improved public health responses in the affected areas, noting the challenges posed by ongoing outbreaks and the populations most vulnerable to severe illness.
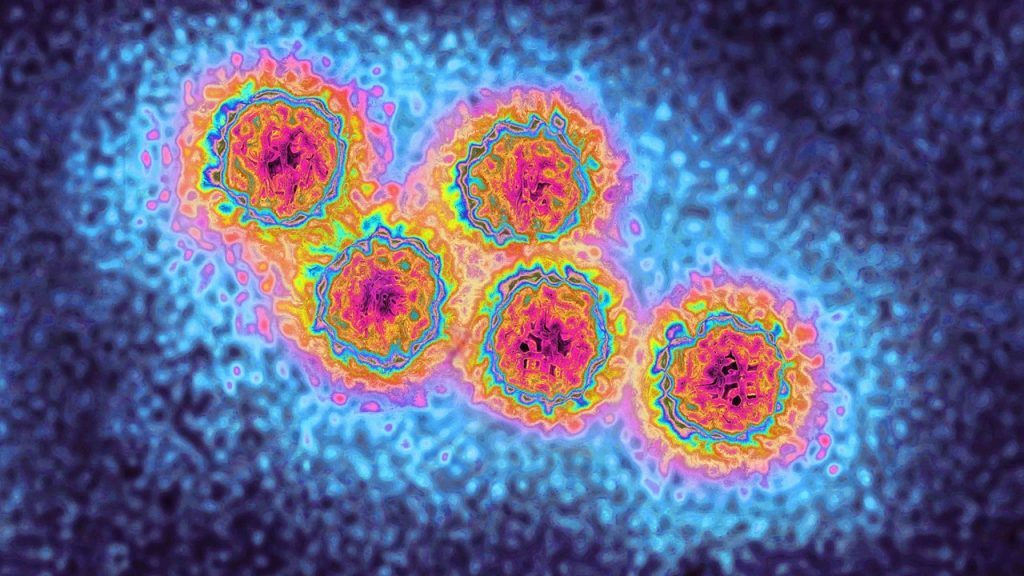
Understanding Hepatitis A
Hepatitis A is an acute viral liver disease transmitted primarily through contaminated food or water, as well as through close contact with infected individuals. According to health officials, the hepatitis A virus (HAV) is highly transmissible, particularly among food handlers. Dr. Marc Siegel, a health analyst, emphasized the virulence of the virus, stating that it “can get you very sick” if contracted.
Vaccination against hepatitis A typically requires two doses taken six to twelve months apart, ensuring that individuals build sufficient immunity. This disease also poses a risk to those who lack access to clean water and good hygiene, often exacerbating its spread among vulnerable populations.
At-Risk Populations
The outbreak has disproportionately affected certain demographics, particularly those who are homeless, inject or use recreational drugs, or live in unsanitary conditions. Individuals within these groups face varying levels of risk, with those under 40 years of age being assessed as moderately at risk, whereas adults over 40 are categorized as high-risk due to the disease’s increased severity with age.
The ECDC has indicated that immunosuppressed individuals and those with pre-existing liver conditions are also susceptible to more severe complications arising from hepatitis A infections. Overall, the risk to the broader general population in these nations has been assessed as low to moderate, albeit with significant concern for high-risk groups.
Response Measures by Health Authorities
In light of the alarming rise in cases, health authorities are ramping up efforts to address the hepatitis A outbreak. The ECDC has recommended targeted vaccination programs aimed at high-risk groups and the implementation of post-exposure prophylaxis for individuals who have had close contact with confirmed cases. Enhanced genetic testing of the virus is also on the agenda to trace its transmission path more effectively.
Ole Heuer, head of the ECDC’s One Health Unit, pointed out the necessity of improving public health outreach, stating that it is crucial to provide access to vaccination and ensure basic sanitation, particularly in areas facing outbreaks. Improved education and increased awareness amongst high-risk populations are essential for mitigating the spread of hepatitis A.
The Importance of Vaccination and Awareness
The continued spread of hepatitis A underscores the critical need for public health campaigns focusing on vaccination and proper hygiene practices. Receiving the hepatitis A vaccine or immune globulin within two weeks of exposure significantly reduces the chances of illness. Health officials emphasize that good sanitation is vital to prevent future outbreaks.
As the outbreak expands, the importance of vaccines cannot be overstated. Individuals who have had the virus develop lifetime immunity, making vaccination a key preventive measure in high-risk groups. Enhanced awareness, particularly regarding symptoms such as jaundice, fatigue, and nausea, allows individuals to seek medical attention promptly, thereby preventing further transmission.
| No. | Key Points |
|---|---|
| 1 | A total of 2,097 hepatitis A cases reported in four European countries. |
| 2 | Slovakia has the highest cases, with 880 infections documented. |
| 3 | Vaccination and sanitation are crucial in controlling the outbreak. |
| 4 | High-risk populations include the homeless and those with limited healthcare access. |
| 5 | Increasing awareness and education among communities is essential for prevention. |
Summary
The emergence of hepatitis A outbreaks in Europe highlights the persistent challenges facing public health systems, particularly among vulnerable populations. As thousands of individuals grapple with the repercussions of this infectious disease, health authorities are taking decisive steps to enhance vaccination efforts and promote hygienic practices. The ongoing response reflects the importance of preparedness and the need for comprehensive public health education, ensuring that communities remain vigilant against future outbreaks.
Frequently Asked Questions
Question: What preventive measures are in place to combat hepatitis A outbreaks?
Preventive measures include targeted vaccination programs, public education about hygiene, and timely access to medical treatment for high-risk populations.
Question: How can hepatitis A be transmitted?
Hepatitis A is primarily spread through contaminated food or water, as well as through close contact with an infected person.
Question: Who is most at risk for severe hepatitis A illness?
Individuals who are homeless, inject drugs, or have pre-existing health conditions, as well as those over 40 years of age, are at a higher risk of severe illness from hepatitis A.