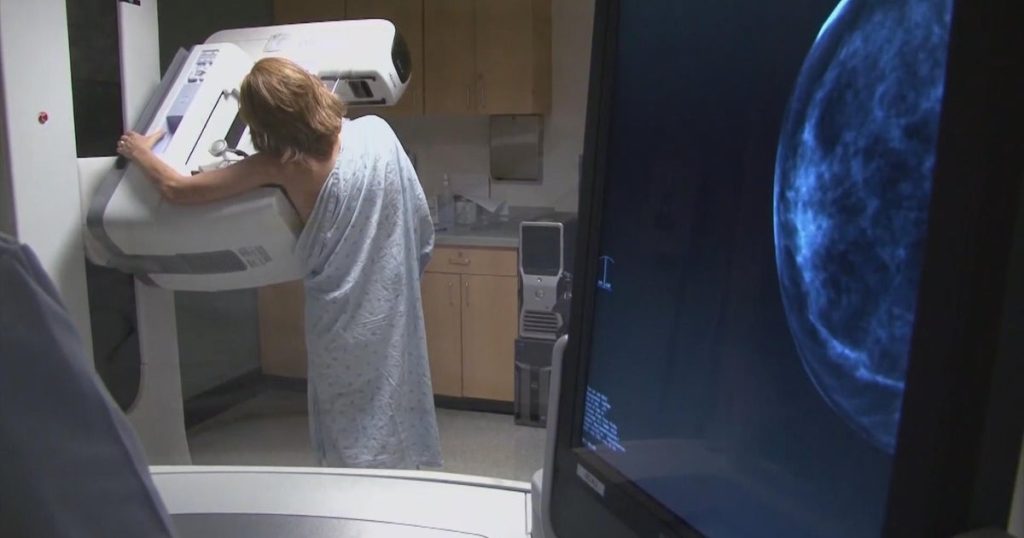
In the United States, over 30 million women undergo mammograms annually, a crucial procedure for early detection of breast cancer. Although many assume these screenings are fully covered by insurance due to the provisions in the Affordable Care Act (ACA), unexpected bills can arise, especially for follow-up tests. A growing number of women are sharing their experiences of unexpected costs, prompting discussions on the need for greater transparency and insurance coverage for additional screenings.
| Article Subheadings |
|---|
| 1) The Reality of Mammogram Costs |
| 2) Real Stories from Affected Women |
| 3) The Role of Insurance and Legislation |
| 4) Impacts of Dense Breast Tissue |
| 5) The Call for Change |
The Reality of Mammogram Costs
Annual mammograms are a key component of women’s health care, primarily designed to detect breast cancer at its earliest stages. Under the Affordable Care Act, women aged 40 and over are entitled to receive these screenings without any out-of-pocket expenses every one to two years. Despite this, many women are discovering that necessary follow-up tests or additional procedures may not be covered, leading to significant unexpected bills.
The ACA aimed to reduce the financial burden associated with preventative health services. However, many insurance plans contain clauses that exclude certain diagnostic procedures, based on the initial mammogram findings. This gap in coverage places an unnecessary burden on many women, who find themselves navigating complex insurance policies after receiving distressing news related to potential health issues.
Real Stories from Affected Women
Stories from women across the country underscore the widespread issue of unexpected medical bills following mammograms. For instance, Sonya Johnson from Topeka, Kansas, expressed her sheer shock after being charged $646 for follow-up ultrasounds due to her dense breast tissue. “I didn’t even think I was going to get charged,” she noted. The emotional rollercoaster of potentially receiving bad news was exacerbated by the financial implications of the diagnostic follow-ups.
Similar accounts emerge from other states, including a woman in Maryland who incurred a $350 charge for extra tests and another in California who faced a $912 bill. The consensus among these women is the lack of transparency regarding what is covered under standard insurance policies, especially concerning additional follow-up tests when mammograms reveal abnormalities.
The Role of Insurance and Legislation
Insurance companies often cite the need for specific medical necessity as the reason behind non-coverage of follow-up tests. However, this reasoning leaves many women in a difficult position. Pat Halpin-Murphy, president of the Pennsylvania Breast Cancer Coalition, emphasized the need for clarity regarding the cost associated with additional testing: “Some women are charged for these tests without knowing that it’s not covered by their insurer.” This void informs the disconnection between women’s health needs and insurance policies.
In response to these growing concerns, legislation has been proposed in Pennsylvania that would require insurers to cover essential follow-up screenings, such as ultrasounds and MRIs, for women with dense breast tissues or other risk factors associated with breast cancer. If enacted, this legislation could prevent many women from being faced with exorbitant bills related to necessary health checks, allowing them to focus on their health rather than their finances during an already stressful time.
Impacts of Dense Breast Tissue
Dense breast tissue is a condition where breast tissue appears white on mammograms, potentially masking tumors that appear darker. It is estimated that about 40% of women undergoing mammography have dense breasts, increasing the chance of missed cancers by more than 50%. For these women, additional screening methods such as 3D mammograms, ultrasounds, or MRIs may be necessary to detect potential issues effectively.
This added complexity means that many women are left to ponder whether they might have cancer, with the pressure to act often leading them to pursue follow-up tests without fully understanding the potential costs involved. The lack of widespread awareness about these costs can hinder access to vital health care for women, contributing to a healthcare environment that disproportionately impacts those with dense breast tissue.
The Call for Change
The growing narrative surrounding the unexpected costs of follow-up tests has ignited a wider discussion about healthcare transparency and the need for reform. Advocacy groups and health organizations are pushing for legislative changes to ensure that insurance plans cover necessary additional screenings without imposing heavy financial penalties on patients. “If this is my preventative care and it’s supposed to be part of my insurance, no, I should not be charged for it,” stated Sonya Johnson, echoing sentiments shared by many others affected.
Moreover, while some organizations provide financial assistance to women affected by these unexpected charges, the work of advocacy groups highlights a critical need for policy change to protect patients and ensure adequate healthcare coverage. Without legislative changes, numerous patients may continue to face significant financial burdens for essential diagnostic screenings.
| No. | Key Points |
|---|---|
| 1 | Over 30 million women receive mammograms annually, yet many face unexpected costs for follow-up tests. |
| 2 | The Affordable Care Act provides mammograms at no cost, but additional diagnostic tests may not be covered. |
| 3 | Women with dense breast tissue often require follow-up imaging, leading to increased bills. |
| 4 | Legislation in Pennsylvania aims to cover essential follow-up screenings, providing needed support for women. |
| 5 | Advocacy groups emphasize the need for healthcare transparency and coverage to prevent financial distress in patients. |
Summary
The issue of unexpected mammogram follow-up charges highlights a significant gap in the insurance coverage landscape for women’s health. With many women receiving alarming news from their initial screenings, the financial repercussions of necessary follow-up tests can lead to unnecessary stress and anxiety. Greater transparency in healthcare billing and stronger legislative measures could help ensure comprehensive coverage for all women, securing their health without the added burden of financial strain.
Frequently Asked Questions
Question: What happens if a mammogram shows an anomaly?
If a mammogram reveals an anomaly, healthcare providers typically recommend additional imaging tests such as ultrasounds or MRIs to determine if it is benign or a potential cancer diagnosis.
Question: Are follow-up tests always covered by insurance?
Not always; the coverage of follow-up tests depends on various factors, including insurance policies and the medical necessity of the tests as determined by the healthcare provider.
Question: How can women advocate for better insurance coverage for mammography-related costs?
Women can advocate for better insurance coverage by joining advocacy groups, contacting their legislators, and sharing their personal experiences to highlight the need for change in health care policies.